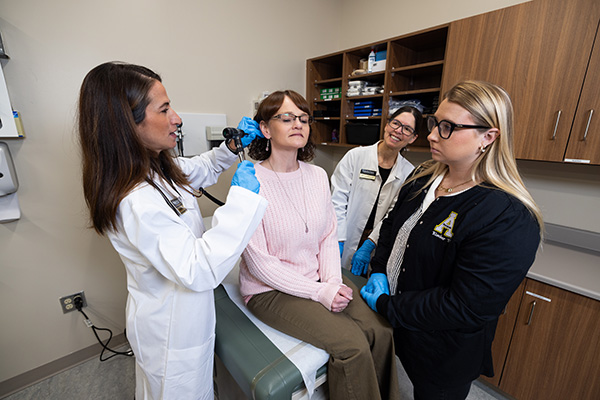
Appalachian State University senior Ashley White, an athletic training major from Arden, left, participates in a simulated clinical scenario depicting a mock injury. These simulations, officially known as Objective Structured Clinical Evaluations (OSCEs), increase students’ confidence, prepare them for independent clinical practice and allow them to gain experience as the lead clinician. In this scenario, Megan Beach, a junior exercise science major from Morganton, right, plays the role of the "patient," pretending to be a high school cheerleader who sustained an open fracture on her lower leg during a stunt. In the role of athletic trainer, White simulated contacting Emergency Medical Services, controlling the bleeding and splinting the broken leg while keeping the patient calm to reduce risk of shock. Photo by Marie Freeman
BOONE, N.C. — Athletic training students at Appalachian State University recently put their skills to the test during a series of simulated clinical scenarios that took place on-site at the university’s Leon Levine Hall of Health Sciences on April 12.
The scenarios, which were not disclosed to the students ahead of time, included:
- A patient overdosing on pain medication.
- A football player with a severe neck injury.
- A patient with a knee injury whose father simultaneously goes into cardiac distress.
- A patient with an open leg fracture.
- A patient with a case of appendicitis.
- A patient having an allergic reaction to a bee sting.
These simulations, officially known as Objective Structured Clinical Evaluations (OSCEs), increase students’ confidence, prepare them for independent clinical practice and allow them to gain experience as the lead clinician in a situation — a distinct experience for a student, said App State’s Laurie Rivera ’97, lead coordinator for OSCEs.
“My favorite part of the simulation is seeing students grow as clinicians and become more confident in their skills. The students enjoy the realism of the cases and the ‘surprises’ that arise,” said Rivera, who also serves as coordinator of clinical education and a senior lecturer in App State’s Master of Science in athletic training program.
Appalachian State University senior Audi Mendoza, an athletic training major from Hendersonville (center, kneeling), participates in a simulated clinical scenario depicting a mock injury. In this scenario, one of Mendoza’s student peers plays the role of the “patient,” pretending to be a 24-year-old arena football player who is found lying unconscious following a tackle during practice. The “patient” regained consciousness but, in the simulation, had numbness and tingling in his arms and legs. Mendoza, in her role as athletic trainer, simulated triaging the situation and determined that spine boarding was appropriate. Photos by Marie Freeman
Nine students participated in the simulations. Graduate students completed all six scenarios, while undergraduate students completed three to four scenarios.
OSCEs are hosted by the Department of Health and Exercise Science multiple times a semester for undergraduate and graduate students, according to Rivera, who shared the university is in the process of phasing out its bachelor’s degree in athletic training.
Undergraduate students have the option to earn a Bachelor of Science in exercise science and an M.S. in athletic training through App State’s Accelerated Admission program or complete a bachelor’s degree of their choice and then apply to the graduate program.
Educational benefits
Each student’s performance in the OSCEs was timed and filmed, and students recorded video reflections after completing their simulations. In the days following the event, faculty reviewed the videos to evaluate competency and provided feedback to the students. The students also watched their own videos and identified strengths and weaknesses.
“OSCEs are an invaluable experience and something that I believe truly sets App State’s athletic training program apart,” said Lauren Morris, an athletic training graduate student from Troy who participated in the event. “I learned from this experience that when I am placed in a similar situation where the stakes are much higher, I have the ability and experience to provide efficient and appropriate medical care.”

Appalachian State University senior Jenny Blackburn, an athletic training major from Oak Ridge, left, participates in a simulated clinical scenario depicting a mock illness. In this scenario, Kevin Mathew, a junior from Charlotte majoring in exercise science, right, plays the role of the “patient,” pretending to be a 20-year-old collegiate soccer player complaining of abdominal pain. In this simulation, the “patient” was alert, in obvious discomfort and anxious about being sick for fear of letting his team down. In her athletic trainer role, Blackburn simulated evaluating the “patient’s” abdomen. She determined appendicitis was the likely diagnosis and a referral to the emergency department at the local hospital would be in order. Photo by Marie Freeman
Rivera said in addition to clinical skills, the students learn how to:
- Triage injuries.
- Communicate with and educate patients.
- Communicate with coaches, administrators and/or guardians when the patient is a minor.
- Coordinate and communicate with Emergency Medical Services (EMS) and other health care professionals.
Emily Gumowitz, a senior from Wellington, Florida, majoring in athletic training who participated in the OSCEs, said these simulations create a neutral ground where students can practice integrating the information they learn in the classroom with the information they learn in a clinical setting.
Gumowitz, who participated in her first App State OSCE in 2019, said she recently re-watched her first post-OSCE reflection video and it made her realize “how much my confidence, knowledge and skills have improved” as a result of these events.
Appalachian State University graduate student Lauren Morris, an athletic training major from Troy, left, participates in a simulated clinical scenario depicting a mock drug overdose. In this scenario, senior Jeremy Bowles, an exercise science major from Charlotte, right, plays the role of the “patient,” pretending to be a 21-year-old collegiate hockey player who recently had a career-ending hip surgery and was found unresponsive in his hotel room by teammates. In her role as athletic trainer, Morris simulated assessing the “patient” and the scene and contacting Emergency Medical Services. She then simulated administering naloxone — used to treat overdoses, along with monitoring and providing care until EMS (also simulated) arrived. Photos by Marie Freeman
Setting the scene
Rivera said the planning for an OSCE begins weeks in advance and includes developing the scenarios and coordinating actors to play patients and bystanders.
Athletic training faculty members write a case file for each simulation that includes:
- A description of the scenario.
- A backstory for the patient.
- An opening vignette that is shared with the student at the start of the scenario.
- A list of materials needed for the scene.
- The associated educational objectives.
The faculty worked to make every aspect of the simulation as realistic as possible. For example, if the student determined they needed to call 911 as part of the scenario, they were handed a card with a phone number that connected them to a faculty member playing a 911 operator.
Appalachian State University student Blair Anderes ’19, a graduate student from Charlotte majoring in athletic training who also earned an App State degree in exercise science, right, participates in a simulated clinical scenario depicting mock medical conditions. In this simulation, Anderes had to prioritize two concurrent “patients.” Harley Tremain, a junior from Collettsville majoring in exercise science, left photo, played the role of the first “patient,” pretending to be a high school baseball player who was hit in the knee with a baseball. During Anderes’ simulated evaluation of the “patient,” Nathan Hambrick, a senior exercise science major from Cary, right photo —playing the role of the “patient’s” father, simulated collapsing with mock chest pain while exercising nearby. In her role as athletic trainer, Anderes simulated triaging the situation and contacting Emergency Medical Services (EMS). Anderes simulated administering medication, monitoring the father and son and transferring care to EMS upon arrival. Photos by Marie Freeman
The patients were played by App State students in the athletic training course Standardized Patients in Healthcare. The course teaches students about the role of simulations in health care education as well as how to draft clinical scenarios and apply moulage (fake injuries).
Gumowitz said she began participating in OSCEs her sophomore year, in the role of a patient, and it provided her a valuable opportunity to “see how the students above me handled situations and to see firsthand what the nature of an OSCE would be like.”
“At previous simulations, students said the scenarios are more realistic when they don’t personally know the individuals involved,” Rivera said.
In response, Rivera recruited athletic trainers from App State Athletics and the M.S. Shook Student Health Service Injury Clinic to play other roles within the scenarios, such as a parent or a coach. Additional actors were recruited from other athletic training courses and the Exercise Science Club to portray bystanders.
What do you think?
Share your feedback on this story.
About the Beaver College of Health Sciences
Appalachian State University’s Beaver College of Health Sciences (BCHS), opened in 2010, is transforming the health and quality of life for the communities it serves through interprofessional collaboration and innovation in teaching, scholarship, service and clinical outreach. The college enrolls more than 3,600 students and offers 10 undergraduate degree programs, nine graduate degree programs and four certificates across seven departments: Kinesiology, Nursing, Nutrition and Health Care Management, Public Health, Recreation Management and Physical Education, Rehabilitation Sciences, and Social Work. The college’s academic programs are located in the Holmes Convocation Center on App State’s main campus and the Levine Hall of Health Sciences, a state-of-the-art, 203,000-square-foot facility that is the cornerstone of Boone’s Wellness District. In addition, the college supports the Appalachian Institute for Health and Wellness and has collaborative partnerships with the Wake Forest University School of Medicine’s Physician Assistant Program, UNC Health Appalachian and numerous other health agencies. Learn more at https://healthsciences.appstate.edu.
About Appalachian State University
As a premier public institution, Appalachian State University prepares students to lead purposeful lives. App State is one of 17 campuses in the University of North Carolina System, with a national reputation for innovative teaching and opening access to a high-quality, cost-effective education. The university enrolls more than 21,000 students, has a low student-to-faculty ratio and offers more than 150 undergraduate and 80 graduate majors at its Boone and Hickory campuses and through App State Online. Learn more at https://www.appstate.edu.